
Posttraumatic Stress Disorder
In the form of Frequently Asked Questions
See also: PTSD and Iraq
Question: What is posttraumatic stress disorder?
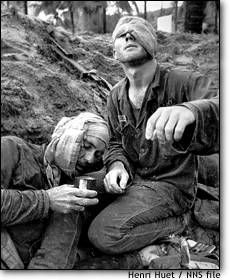
Answer: Posttraumatic stress disorder, usually referred to as PTSD, is a new label, but a timeless disease. The earliest accounts of trauma and war in history and literature give examples of what today would most likely be recognized as posttraumatic stress disorder.[1] In contemporary American culture, we tend to think of the trauma causing posttraumatic stress disorder as combat, but sexual and physical assault, motor vehicle accidents, natural disasters, and other trauma are also potential causes of posttraumatic stress disorder.
Question: How is posttraumatic stress disorder diagnosed?
Answer: An easy mnemonic for posttraumatic stress disorder follows:
ERASE:
Experience: obviously there must be a traumatic experience. Trauma as defined here is quite different from everyday stress, such as the stress of taking an exam. Rather, trauma must include a sense of overwhelming loss of control or a feeling that one is about to die. Survivors will often describe the experience as "this is it" or a "close call." Note that two people can be exposed to the same event and one may experience it as traumatic, whereas the other, perhaps through lack of awareness of the dangers involved, may not. The most common traumas include assault, rape, being held hostage, combat, natural disasters, motor vehicle accidents, and physical or sexual abuse. Note that the posttraumatic stress disorder that arises from childhood abuse has a different flavor than that resulting from a trauma experienced in adulthood after one's personality is more or less formed. Note also that a single trauma is much less likely to cause posttraumatic stress disorder (although it might) than a recurrent pattern of repetitive trauma. United States Army studies in North Africa and Guadalcanal in World War II indicate that 100% of any combat unit become psychiatric casualties after about 60-120 days of continuous, heavy combat. It doesn't mean all will develop posttraumatic stress disorder, but there is a linear relationship between the intensity of the trauma and the prevalence of posttraumatic stress disorder. For example, the prevalence of posttraumatic stress disorder among those who are wounded in action is about 75%.
Reexperiencing: The most common forms of this are through nightmares and flashbacks. The nightmares maybe so intense that a spouse or significant other can't sleep in the bed with the patient out of fear of being hit, kicked, or even strangled. The flashbacks are fleeting but extremely intense sensation that "it's happening again." The person is momentarily transported back to the trauma. It can be viewed as a dissociative phenomenon. Less dramatic but more common are recurrent, intrusive, unwanted thoughts of the trauma. Patients will go to incredible extremes to avoid these thoughts and the resultant flood of feelings.
Avoidant behavior: This can be subtle but usually involves staying away from something that reminds the patient of the trauma, especially something that triggers reexperiencing. This can be anything from the sound of a helicopter to avoiding watching the news because of the violence. Many combat veterans will tell you they could never watch war movies or violent films again (John Wayne was booed off the stage by battle-hardened Marines during a World War II USO tour). Patients may also avoid crowds, people, relationships, or their own feelings. The result maybe described as a numbness or a shutting down of their emotions. Obviously, this can wreak havoc in a relationship. This urge to avoid may come and go and maybe especially intense around the "anniversary period" of the trauma, e.g., January for Tet Offensive survivors, or the date a patient was wounded. Patients may isolate socially, sometimes going to the extreme of living in the woods, leaving without notice, disappearing for a few days or weeks.
Sympathetic Excess: If you can imagine your feelings if a man with a knife stepped out in front of you in a dark alley, you can get a taste of what this is like. The posttraumatic stress disorder patient has an outpouring of catecholamines triggered by a much lower stimulus than controls. They can be jumpy like a cat, flinching at a backfiring car, or ducking or throwing themselves to the ground after certain overwhelming stimuli.
Question: Are there other posttraumatic stress disorder symptoms?
Answer: Yes, there are several.
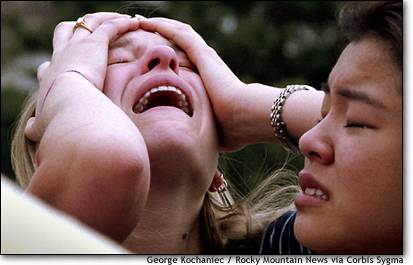
Survivor guilt is common and is a literal feeling of shame or guilt that they survived when others didn't. This is a very intense, visceral experience. Patients may be able to recognize that it is irrational or overvalued, but they experience it nevertheless.
Difficulty with trust: this seems especially true of the Vietnam generation, who were betrayed in many ways, but is true to a certain extent of any trauma survivor. Most of us trust that the world is a relatively safe, predictable place. Trauma survivors know it isn't, so don't tend to be as trusting. They may have a sense that something terrible will happen if they let down their guard.
Mood swings: posttraumatic stress disorder is often misdiagnosed as bipolar disorder. Interestingly, the treatment for each is similar (both respond to mood stabilizers, such as lithium or valproic acid). These mood swings may include impulsivity and rage attacks. Always ask about violence.
Substance abuse: substance abuse is very common among posttraumatic stress disorder patients, probably representing an attempt to self-medicate. Many will describe drinking themselves to sleep, for example, attempting to blot out nightmares.
Existentialist Angst: by this I mean that the posttraumatic stress disorder patient's world outlook may have been fundamentally shattered by the trauma, especially if it was random (as most trauma is). We are led to believe that if we follow the rules (eat the right foods, fasten our seatbelts, don't smoke), bad things won't happen to us, but when terrible things happen to good people with regularity, it can destroy a person's belief system. This is often one of the most painful aspects of posttraumatic stress disorder, a sense that the universe is a hostile, unpredictable, violently random place.
Question: How common is posttraumatic stress disorder?
It varies from culture to culture based generally on exposure to stress. Although the syndrome was recognized and formally categorized in the West, it has been seen cross culturally from Vietnam to Cambodia to Mozambique to the West Bank and Gaza.
The United States has a low level of posttraumatic stress disorder compared to many developing countries, but a higher rate compared to other industrialized nations. Between 7.9 and 8.7% of the American population suffers from posttraumatic stress disorder (source: Davidson et al 1991 (7.9%), Breslau et al 1991 (8.7%), Kessler et al, 1995 (7.8%)).
Have the events of September 11, 2001, led to a dramatic increase in posttraumatic stress disorder rates in the United States?
Not really. As with any disaster or catastrophe, those closest to the event suffered the greatest trauma. For example, school children in Manhattan who witnessed people falling from the World Trade Center had higher rates of posttraumatic stress disorder than children who didnít. Geographically, posttraumatic stress disorder rates were higher in lower Manhattan and parts of New Jersey (where many of those who worked in the buildings lived) than in other parts of the country.
The other reason posttraumatic stress disorder rates did not skyrocket post-9/11 is because the United States has a relatively high rate of violence. Approximately 5 times as many Americans were murdered by other Americans in 2001 than died as a result of the 9/11 attacks (and the homicide rate in 2001 was lower than in the recent past). If we imagine that for every homicide there are several hundred or thousand assaults, then the number of victims of violence is quite large, much larger than in other industrialized countries. Each violent episode has the potential to create several cases of posttraumatic stress disorder.
Question: If violence is a major source of trauma, then which groups suffer from the highest rates of violent death?
The per capita violent death rate for the groups involved follow:
|
Group: |
Rate per 100,000 per year: |
Bar graph (+ = 50/100,000) |
|
Homicide rate African American males, age 15-24* |
167 |
+++++++++++++++++ |
|
Homicide rate all American males, age 15-24* |
40 |
++++ |
|
Homicide rate all Americans* |
7.9 |
++ |
|
9/11 per capita death rate**: |
1.0 |
. |
|
Israeli violent death rate since 9/00:*** |
- |
|
|
Palestinian violent death rate since 9/00:*** |
++ |
|
|
Japanese homicide rate |
<1 |
. |
* source: US Department of Justice, FBI, CDC; year 2000 data used; ** annualized as of 11/02; 2001; *** annualized for the period 9/02-11/02 (last updated 11/12/02).
This table mixes apples and oranges to a certain extent, but gives a crude idea of the order of magnitude difference between violent death rates between some selected groups.
Question: Has posttraumatic stress disorder been studied in other cultures?
Yes. The prevalence is much higher among populations that suffer much higher background rates of trauma, such as Palestinian children:
Rates of POSTTRAUMATIC STRESS DISORDER in high risk populations:
|
Palestinian children |
73% |
|
Bosnian refugees |
65% |
|
Kosovo community |
17% |
- Sources (in order): Thabet and Vostanis, 1999; Weine 1995, Cardozo 2000.
Question: Neurobiologically, what causes the symptoms of posttraumatic stress disorder?
Answer: The easiest way to remember posttraumatic stress disorder is that it is most likely a resetting of the hypothalamic-pituitary-adrenal axis, such that someone exposed to intense trauma requires far less subsequent stimulation to induce a fight-or-flight response with all the attendant physiological arousal, and takes longer to return to baseline. Like panic disorder patients (it is important to remember that posttraumatic stress disorder is an anxiety disorder), posttraumatic stress disorder patients will avoid anything that might trigger this intensely painful physiological response, usually visual, acoustic, and even olfactory cues that remind them of the trauma. For example, some Vietnam combat veterans can experience a flashback - an intense reliving of their traumatic experience - when exposed to the smell of rice.
Question: What evidence is there of a neurobiological basis of posttraumatic stress disorder?
Answer: There are several pieces of evidence. One of the most interesting involves a brain structure called the hippocampus. Researchers who measure hippocampus volume via MRI (magnetic resonance imaging) have demonstrated a 15% shrinkage in those with posttraumatic stress disorder versus those without. Whether the shrinkage in the hippocampus precedes the trauma (and therefore predisposes to the development of posttraumatic stress disorder) or follows (and is a result of) the trauma is unclear. Some twin studies indicate that of 2 twins, the 1 with the smaller hippocampus before a trauma is more likely to go on to develop posttraumatic stress disorder given exposure to a trauma. Other studies, however, show that successful posttraumatic stress disorder treatment may lead to an increase in the hippocampus. (source: Bremner, 1995; Bremner 1997). [2]
Question: Is there a time requirement for diagnosing posttraumatic stress disorder?
Answer: Yes with DSM-4, although DSM-5 may change this. Posttraumatic stress disorder cannot be diagnosed until 1 month after the trauma. Why does this matter? Because the majority of people exposed to a trauma will develop some posttraumatic stress disorder symptoms (nightmares, reexperiencing, intrusive thoughts), but most will NOT develop posttraumatic stress disorder (depending on the intensity of the trauma). They may have some residual symptoms, but most will muddle through. Sometimes patients do fine during their working life, distracting themselves perhaps, but then decompensate during retirement. It can have a very delayed onset, in other words.
Question: Is posttraumatic stress disorder overdiagnosed?
Answer: probably not. There is strong evidence that posttraumatic stress disorder if anything is under-diagnosed. It is critical to ask all patients with mood disorders or any possible posttraumatic stress disorder symptoms for a trauma history, particularly history of assault or sexual abuse. Only about 2% of posttraumatic stress disorder gets diagnosed in a primary medical setting. Psychiatrists don't do much better: 4% of community psychiatrists and 14% of academic psychiatrists made the diagnosis of posttraumatic stress disorder appropriately.
Question: Do patients with posttraumatic stress disorder develop other psychiatric conditions (co-morbidity)?
Answer: Yes. The percent prevalence for various psychiatric conditions in patients with and without posttraumatic stress disorder follows:
|
Psychiatric |
Posttraumatic Stress Disorder |
Non-posttraumatic stress disorder |
|
Generalized anxiety disorder |
53% |
9 |
|
Major depression |
30 |
4 |
|
Somatization |
12 |
0 |
|
Substance abuse |
9 |
1 |
Interestingly, posttraumatic stress disorder patients also have higher % prevalence rates of medical morbidity:
|
Medical: |
Posttraumatic Stress Disorder |
Non-posttraumatic stress disorder |
|
Asthma |
13 |
5 |
|
Peptic ulcer disease |
13 |
4 |
|
Hypertension |
31 |
18 |
Question: What is the medication treatment for posttraumatic stress disorder?
Answer: Treatment is usually multidisciplinary and may involve individual and group therapy, particularly helpful if done with other survivors of the same type of trauma, such as World War II combat support groups, and medication.
Treatment of posttraumatic stress disorder should be multi-disciplinary (psychotherapy and medication management).
Medication mangement:
Serotonergic agents: the first antidepressant to be shown to be effective in the treatment of posttraumatic stress disorder was sertraline. In placebo-controlled trials, about 60% of those suffering from posttraumatic stress disorder responded when treated with sertraline, versus 40% for placebo. The mean dose of response was 151.3 mg for those who completed the study. (Source: Brady, 2000, Davidson, 2001).
To illustrate how difficult posttraumatic stress disorder is to treat, response is considered a 30% improvement in the CAPS score (versus 40% for schizophrenia and 50% for major depression).
Patients tend to improve in the first few weeks, but treatment does not differentiate significantly from placebo until week 12.
Other selective serotonin reuptake inhibitors such as paroxetine and fluoxetine have also been shown to be superior to placebo in the treatment of posttraumatic stress disorder. Not only do these medications reduce symptoms, but they appear to decrease psychosocial impairment, as measured by the Sheehan Disability Scale (SDS) (source: Tucker, 2001).
Other antidepressants that have been shown effective in posttraumatic stress disorder include nefazodone and perhaps lamotrigine. Wellbutrin is most likely not effective in posttraumatic stress disorder.
Many clinicians believe that mood stabilizers such as the anticonvulsants (Depakote or Tegretol) or lithium should be the mainstay of posttraumatic stress disorder treatment, but unfortunately there are no controlled trials in posttraumatic stress disorder demonstrating their superiority over placebo.
Other useful medications include hypnotics to help with sleep or to take as needed for anxiety, such as benzodiazepines. Although one must be cautious in the posttraumatic stress disorder, population, especially with males, regarding substance abuse and dependence, the proportion of patients who abuse benzodiazepines is very small. Note, however, that acute administration of benzodiazepines following a trauma to survivors with high levels of initial distress to not have a "salient beneficial effect on the course of their illness" (Gelpin, 1996).
Beta blockers such as propranolol has been shown to decrease the physiological hyperarousal of posttraumatic stress disorder (Pitman, 2002).
Multiple drug classes are the rule, not the exception.
Question: What about psychotherapy for posttraumatic stress disorder?
Answer: Several approaches have good data to support their use. A few do not, or have even been shown to be harmful.
Supportive treatment, especially in a group format of others who have experienced similar trauma, may be helpful. Group therapy has been demonstrated to be effective in the treatment of posttraumatic stress disorder.
Psychosocial debriefing, typically a 15-45" session closely following a trauma, has been shown to be worse than no intervention at all unless followed by subsequent intervention.
Cognitive behavioral therapy can be useful, especially to deal with cognitive distortions around issues such as survivor guilt.
Virtual Reality: Another exciting area is that of exposure therapy using Virtual Reality techonology. Click here for a CNN story covering the VR treatment at the Atlanta VAMC. Exposure therapy in combination with sertraline may be more effective by week 15 than either treatment alone (source: Rothbaum, Davidson, 2002).

There is little data to support the use of psychodynamic treatment in posttraumatic stress disorder.
Question: What is the cost of NOT treating posttraumatic stress disorder?
Answer: posttraumatic stress disorder should be thought of as an illness that has a significant lifetime cost if untreated. The average number of posttraumatic stress disorder episodes suffered by an individual with posttraumatic stress disorder is 3.3; the average duration of each episode is 7.0 years. The typical person with posttraumatic stress disorder has over 20 years of active symptoms. (Source: Breslau, 1998, Kessler, 2000). Economically, posttraumatic stress disorder is estimated to cause an average work loss = 3.6 days/ month and an annual productivity loss of $3 billion
Endnotes
[1] An excellent book illustrating this is Jonathan Shay's Achilles in Vietnam: Combat Trauma and the Undoing of Character, written by a VA psychiatrist comparing the narrative of his Vietnam combat veterans with the narrative of Homer's Iliad. If you want to grasp the essentials of this disorder, read this book.
[2] Note also that increased glucocorticoids and a decrease in BDNF, all of which can be caused by trauma, has been shown to cause atrophy and death of neurons -> shrinkage of hippocampus. Antidepressants can lead to increase in serotonin and norepinephrine and increase in BDNF and decrease in glucocorticoids which in turn can lead to an increase in survival and cell growth; - source: Duman, Heninger & Nestler 1997.