Posttraumatic Stress Disorder
See also: PTSD OverviewWhat is posttraumatic stress disorder?
Posttraumatic stress disorder is a new label, but a timeless disease. The earliest accounts of trauma and war in history and literature give examples of what today would most likely be recognized as posttraumatic stress disorder. An excellent book illustrating this is Jonathan Shay's Achilles in Vietnam: Combat Trauma and the Undoing of Character, written by a VA psychiatrist comparing the narrative of his Vietnam combat veterans with the narrative of Homer's Iliad. If you want to grasp the essentials of this disorder, read this book.
Posttraumatic stress disorder probably has a strong physiological and psychological basis. At the biological level, it can be thought of as a resetting of our normal "stress thermostat" if you will. Someone with posttraumatic stress disorder requires far less subsequent stimulation to induce a fight-or-flight response. Posttraumatic stress disorder patients will avoid anything that might trigger this intensely painful physiological response, including their own strong feelings surrounding the trauma.
An easy mnemonic for posttraumatic stress disorder follows:
ERASE:
Experience: obviously there must be a traumatic experience. Trauma as defined here is quite different from everyday stress, such as the stress of taking an exam. Rather, trauma must include a sense of overwhelming loss of control or a feeling that one is about to die. Survivors will often describe the experience as "this is it" or a "close call." Note that two people can be exposed to the same event and one may experience it as traumatic, whereas the other, perhaps through lack of awareness of the dangers involved, may not. The most common traumas include assault, rape, being held hostage, combat, natural disasters, motor vehicle accidents, and physical or sexual abuse. Note that the posttraumatic stress disorder that arises from childhood abuse has a different flavor than that resulting from a trauma experienced in adulthood after one's personality is more or less formed. Note also that a single trauma is much less likely to cause posttraumatic stress disorder (although it might) than a recurrent pattern of repetitive trauma. United States Army studies in World War II indicate that 100% of any combat unit become psychiatric casualties after about 90 days of continuous, heavy combat. It doesn't mean all will develop posttraumatic stress disorder, but there is a linear relationship between the intensity of the trauma and the prevalence of posttraumatic stress disorder. For example, the prevalence of posttraumatic stress disorder among those who are wounded in action is about 75%.
Reexperiencing: The most common forms of this are through nightmares and flashbacks. The nightmares maybe so intense that a spouse or significant other can't sleep in the bed with the patient out of fear of being hit, kicked, or even strangled. The flashbacks are fleeting but extremely intense sensation that "it's happening again." The person is momentarily transported back to the trauma. It can be viewed as a dissociative phenomenon. Less dramatic but more common are recurrent, intrusive, unwanted thoughts of the trauma. Patients will go to incredible extremes to avoid these thoughts and the resultant flood of feelings.
Avoidant behavior: This can be subtle but usually involves staying away from something that reminds the patient of the trauma, especially something that triggers reexperiencing. This can be anything from the sound of a helicopter to avoiding watching the news because of the violence. Many combat veterans will tell you they could never watch war movies or violent films again Those suffering from posttraumatic stress disorder may also avoid crowds, people, relationships, or their own feelings. The result maybe described as a numbness or a shutting down of their emotions. Obviously, this can wreak havoc in a relationship.
Sympathetic Excess: If you can imagine your feelings if a man with a knife stepped out in front of you in a dark alley, you can get a taste of what this is like. The person suffering from posttraumatic stress disorder has an outpouring of adrenaline triggered by a much lower stimulus. They can be jumpy like a cat, flinching at a backfiring car, or ducking or throwing themselves to the ground after certain overwhelming stimuli.
Are there other symptoms of posttraumatic stress disorder?
Yes, these other symptoms include:
Survivor guilt is common and is a literal feeling of shame or guilt that they survived when others didn't. This is a very intense, visceral experience. Patients may be able to recognize that it is irrational or overvalued, but they experience it nevertheless.
Difficulty with trust: this seems especially true of the Vietnam generation, who were betrayed in many ways, but is true to a certain extent of any trauma survivor. Most of us trust that the world is a relatively safe, predictable place. Trauma survivors know it isn't, so don't tend to be as trusting. They may have a sense that something terrible will happen if they let down their guard.
Mood swings: posttraumatic stress disorder is often misdiagnosed as bipolar disorder. Interestingly, the treatment for each is similar (both respond to mood stabilizers, such as lithium or valproic acid). These mood swings may include impulsivity and rage attacks. Always ask about violence.
Substance abuse: substance abuse is very common among posttraumatic stress disorder patients, probably representing an attempt to self-medicate. Some will use alcohol in an attempt to obliterate memories, usually unsuccessfully.
How can someone tell the difference between being a little "stressed out" and having something more serious that might need treatment or evaluation?
The good news is that the majority of people exposed to a trauma do just fine with time. Many may experience transient symptoms of the syndrome currently known as posttraumatic stress disorder (see below), but over time these symptoms go away or become much less bothersome.
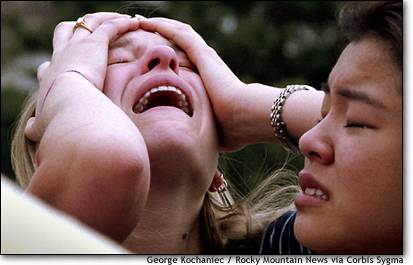
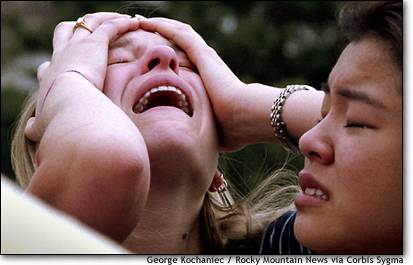
Some, perhaps a third of those with proximity to the trauma, such as those who witnessed it firsthand, who had the experience that they were going to die, or who lost a loved one, will go on to develop posttraumatic stress disorder.
What about the psychological aspect of posttraumatic stress disorder?
Most researchers recognize the role of cognitive changes that occur from trauma. Many trauma survivors suffer from existentialist angst, in which one's world outlook may have been fundamentally shattered by the trauma, especially if it was random (as most trauma is). We are led to believe that if we follow the rules (eat the right foods, fasten our seatbelts, don't smoke), bad things won't happen to us, but when terrible things happen to good people with regularity, it can destroy a person's belief system. This is often one of the most painful aspects of posttraumatic stress disorder, a sense that the universe is a hostile, unpredictable, violently random place.
So when should I consider getting treatment or evaluation if I think I have posttraumatic stress disorder?
Technically, you can't diagnose posttraumatic stress disorder unless symptoms persist for at least a month after a trauma. However, some research indicates that the sooner treatment is obtained, the better. In fact, debriefing trauma survivors almost immediately, in an emergency room setting, for example, may lead to a better outcome.
Remember that the majority of people exposed to a trauma will develop some posttraumatic stress disorder symptoms (nightmares, reexperiencing, intrusive thoughts), but most will NOT develop posttraumatic stress disorder (depending on the intensity of the trauma). They may have some residual symptoms, but most will do fine during their working life.
Who is most at risk of developing posttraumatic stress disorder?
Those most at risk are obviously those most severely traumatized, but also those who have a past history of trauma, particularly of childhood abuse. Also, anyone who was having some difficulties with anxiety or depression prior to a trauma maybe somewhat more vulnerable. But the bottom line is that anyone can develop posttraumatic stress disorder.
If posttraumatic stress disorder is so important, why was the diagnosis only added to the Diagnostic and Statistical Manual in 1980?
Although posttraumatic stress disorder was not formally recognized and codified as an illness as it is currently understood, there is overwhelming evidence that people suffered from what we would now call posttraumatic stress disorder throughout history.
Was there more posttraumatic stress disorder from the Vietnam conflict than from other wars?
No. Although the diagnosis did not exist, the syndrome we would now call posttraumatic stress disorder existed in every war and natural disaster. By some measures, World War II produced more psychiatric casualties than did the Vietnam conflict. After intensive combat in World War II, for example, up to 75% of some units would become psychiatric casualties. The military devoted a tremendous amount of effort to understanding how what was called "shell shock" or "battle fatigue" at various times could be prevented or treated, with only limited success until recently. Notably, no personality tests were able to predict who would most likely become a psychiatric casualty.
Is posttraumatic stress disorder a sign of weakness, or evidence that someone can't cope?
Not at all. Posttraumatic stress disorder is not a sign of weakness, but a physiological inevitability. It makes no more sense to label those with posttraumatic stress disorder as weak than it does to accuse someone with a broken leg of having weak bones. The bravest thing someone with posttraumatic stress disorder can do is to step forward and get treatment. Unfortunately, many donít until they have suffered tremendously.
Is it possible to do OK for awhile, then develop posttraumatic stress disorder?
Yes, posttraumatic stress disorder can have a delayed onset. In fact, those who become completely numb during a trauma, or those who get a strong sense of depersonalization (being out of their body) or derealization ("this isn't really happening") may be more at risk of developing posttraumatic stress disorder later. Talking about what happened - debriefing - appears to be very important.
On one extreme, some people may distract themselves for years, perhaps burying themselves in their work, then do poorly during retirement, when they have more time to think, and old memories come back to haunt them.
So how is posttraumatic stress disorder treated?
The first step is to get a thorough psychiatric evaluation. This should include not just a detailed history and mental status examination, but also in some cases a medical examination. There are some medical conditions that can mimic the anxiety of posttraumatic stress disorder that should be ruled out.
The treatment is usually multidisciplinary, meaning it should involve ideally physicians, psychologists, social workers, individual and group therapy, and possibly medications. Support groups, particularly helpful if done with other survivors of the same type of trauma, such as World War II combat support groups or sexual assault survivors, can be life-savers.
Can medications help?
Definitely. Sertraline (Zoloft) was the first medication to get FDA approval for the treatment of posttraumatic stress disorder, but many others are effective. These include mood stabilizers such as the anticonvulsants (Depakote or Tegretol) or lithium, as well as antidepressant medication, such as fluoxetine or sertraline, and medications to help with anxiety, such as benzodiazepines (medications such as clonazepam or Xanax).
What other areas are helpful?
Some exciting research is being conducted with Virtual Reality. The Atlanta VA Medical Center was using this for Vietnam combat veterans.

Computer-generated helicopter in a virtually created Vietnam.
The idea behind this is that at one level posttraumatic stress disorder is a conditioned response and that exposing someone to the stimuli that accompanied the response (such as the sound of helicopters or small arms fire) without having a bad outcome (such as someone getting wounded or killed) could lead to extinction of the response (that is, the sound no longer might stir up the same intense physiological arousal). Whether a similar exposure might help with the World Trade Center and Pentagon attacks is unclear. If anything, Americans were flooded with images of these events already.
If I don't think I have posttraumatic stress disorder but have a number of disturbing symptoms, what should I do?
Don't overlook the simple things. Be good to yourself. Tune out the stimuli if they are overwhelming. Get your news in less graphic form, such as the printed media, and in measured doses. You probably don't need a minute-by-minute update of what is going on in the world. Focus your energy on things you can control, such as your intimate relationships. Rediscover gardening or some old hobby that used to be soothing and uplifting. Talk to people, but don't overdo it; if you are constantly talking about September 11th, perhaps it's time to expand your circle of friends. And don't forget to get enough sleep, avoid illicit drugs or excessive alcohol, and get plenty of exercise. Eat a balanced diet.
Suppose I try those things and still have symptoms?
Perhaps you should consider a formal evaluation.